(前編を読む)
対策を定着させるのに必要なシンプルなツール
Simple tools are needed to formulate a response
私たち教会は、病気を防ぎ、弱っている人々を保護する大きな役割を持っている。教会は、地域における不可欠な一部であり、多くの社会的接触行為が私たちの教会を介して行われる。新型コロナ・ウイルスが発生した初期の段階で兆候を見逃さなければ、教会内の人々や地域の人々を保護することができる。
しかし、これまで疾病対策に取り組んだ経験から、説得だけでは人々に行動を起こさせるには不十分だと私は知っている。人々が行動を起こすのには、あるシンプルなツールが必要なのだ。
As part of our mission in this world, the church can be a strong agent to prevent sickness and protect the vulnerable. We are an integral part of our community, and many social contacts run through our church. If we can recognize the early signs of a local COVID-19 outbreak, we can lead in protecting those inside and outside our churches. But I have worked with enough disease control efforts to know that it is not enough to convince people they should act. People need to be given simple tools to help them take action.
米国の教会は、この疫病流行への対処法について知らないことが多い。私たちは、この疫病が拡散するのに合わせて、その対処を学んでいる。最近の経験から得た教訓として、教会がすぐに適切な決定を下せるようにする二つの簡単なツールを提案する。
(1)地域の伝染リスク度合いに基づいて、教会がどのような行動を取るべきかを評価する簡単な方法
(2)感染を防ぐため、必要に応じて教会がすぐに実施できる「人との距離を確保する対策」とその計画のための枠組み
Churches in the US are in uncharted territory regarding how to respond to the current epidemic. We will all continue to learn as this epidemic evolves. But based on my recent experience, here are two simple tools to help churches make good decisions in real time: (1) a simple way to assess what kind of actions a church should take based on the local risk of transmission, and (2) a framework that can help churches develop a specific plan to prevent infection and increase social distancing that can be implemented as soon as it is necessary.
教会のリスク判断と対応を決定する方法
How to determine your church’s risk and response
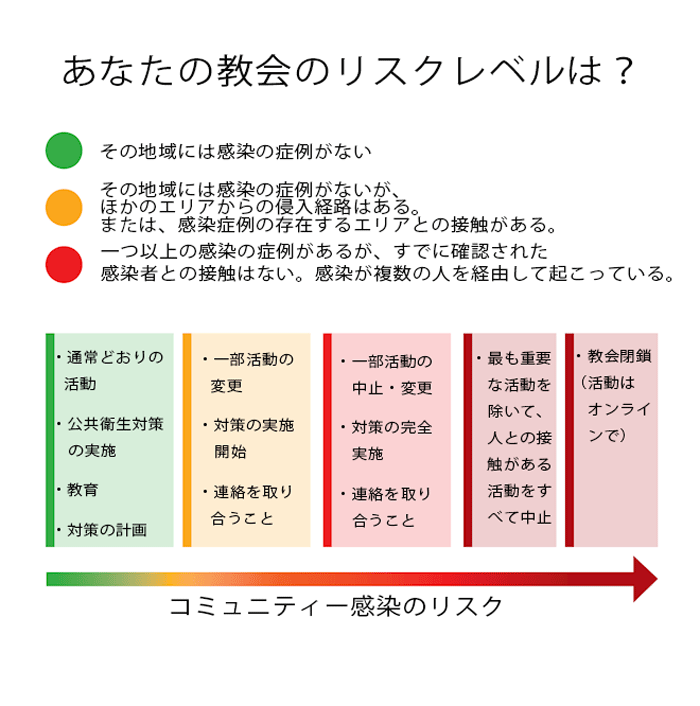
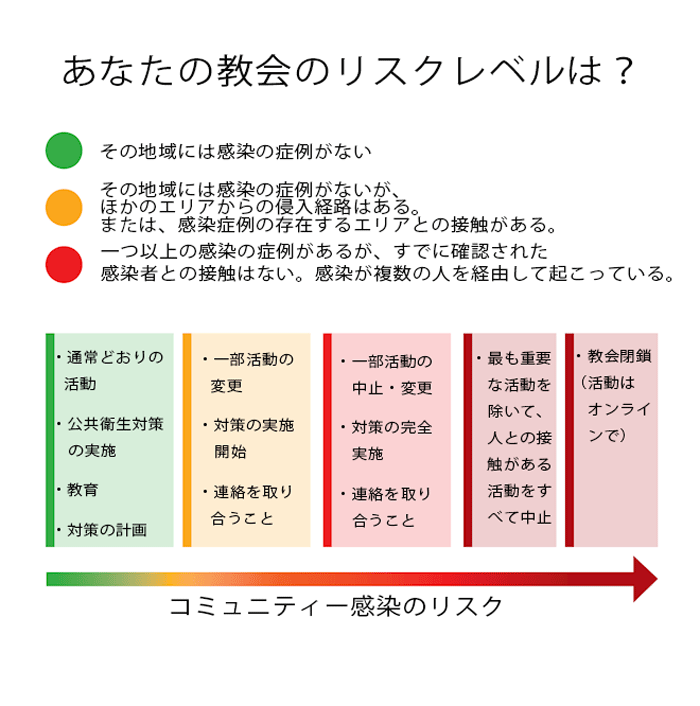
新型コロナ・ウイルスの症例が増加するにつれて、教会がどう対応すべきかについて、多くの不安の声が聞かれる。しかし、必要なのは、疫学の原則に基づいた正しい対応を取ることだ。私は信号機の色を使って、教会が地域の状況に合わせてどのような行動を取るべきかを分かりやすく示した(上図を参照)。結局のところ、このウイルスが広がるのはそれぞれの地域の中でなのだ。遠くで起こっていることに基づいた行動を取るべきではない。大事なのは、その地域で起こっていることに基づいた対策を取ることだ。
As cases of COVID-19 increase, we are seeing a lot of anxiety and uncertainty about what the church should do. But responses can be based on sound epidemiologic principles. I use traffic light imagery to help churches think through their local risk of transmission and what kind of actions they should take (see figure). After all, all transmission of this virus occurs locally. Your actions should not be based on what is happening 50 miles away; they should be based on what is happening in your particular community.
その地域に、新型コロナ・ウイルス感染の症例が報告されていないとき、あなたの教会は「青信号」ゾーンにある。あなたはどのような行動を取るべきだろうか。
Your church is in a “green light” zone when there are no known cases of COVID-19 in your community. What should you be doing?
●自分が病気の時にするような手洗いや十分な休養を取ることなど、一見平凡でも効果のある公衆衛生対策をすべて実施しよう。
Implement all of those boring but effective public health measures like hand-washing and staying home when you are sick.
●新型コロナ・ウイルスについて、その症状、広がり方、高齢者や基礎疾患のある人への影響、感染から身を守るためにできることについて教会員を教育しよう。
Educate your church about the COVID-19—its symptoms, how it spreads, how it affects the elderly and those with chronic illnesses, and what they can do to protect themselves from being infected.
●教会内で話し合いを行い、必要に応じた教会活動の修正、中止、または企画差し替えなど、具体的な計画を立てるべきだ。教会の指導者は、このプロセスに携わる必要がある。この段階は、教会が間もなく直面しうる事態に備えて、基礎を築く大事な時だ。
Carry out discussions within the church and make concrete plans to modify, cancel, or replace church activities as needed. The church leadership should be engaged in this process. Now is the time lay a good foundation in preparation for what the church might face next.
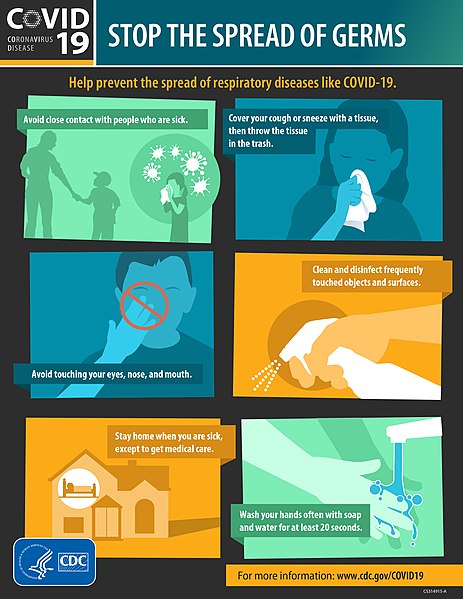
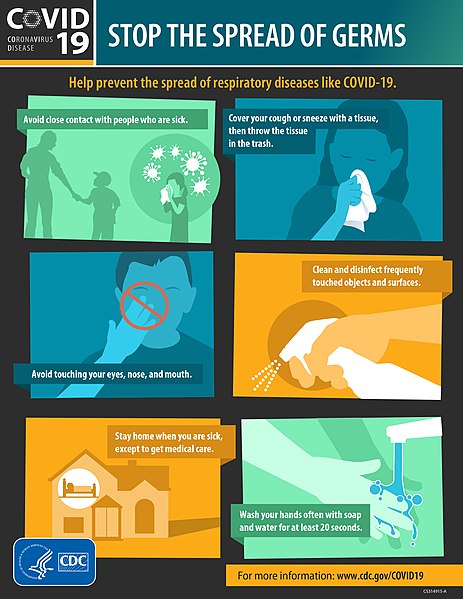
ウイルス拡散を止める方法を説明した米国疾病管理予防センターのポスター
大量の人的移動や旅行が簡単に行えるようになったことで、多くのコミュニティーに新型コロナ・ウイルスが流れ込んでいる。近隣のコミュニティーで感染者が出れば、あなたの教会はすぐ「黄信号」ゾーンに該当することになる。ただし、感染者との接触を持った人が誰も感染していなければ、新型コロナ・ウイルスが発生したとは言えない。感染者との接触を持った一人、あるいは複数人が感染したとしても、コミュニティー内でほかの人に感染していなければ、感染の拡大は起こっていない。教会はまだ黄信号ゾーンだ。この時点で、あなたの教会はどのような対応を取るべきだろうか。
Because of the huge mobility of people and ease of travel, many communities have started to see COVID-19 cases imported into their community. As soon as a case from another community enters your community, your church is in the “yellow light” zone. If no one who came into contact with this case is infected, this indicates there was no further transmission of COVID-19. When one or more of the contacts are infected, but no one else in the community is infected, this means transmission has not spread to the broader community. The church is still in the yellow zone. At this point, what should your church be doing?
●教会が具体的な対策を完全に立案できていなければ、今すぐ対策案を完成させるべきだ。
If your church hasn’t completed a concrete response plan, do it now.
●その対策を実施し、いくつかの活動を修正してリスクを軽減し、そのことを教会全体に知らせよう。
Begin implementing this plan, modifying some activities to reduce risk and inform the entire church about this.
●教会活動の変化を信徒全員に迅速に伝えられるシステムを作る必要がある。
Establish a system to rapidly communicate any changes in church activities to the entire congregation.
●十分な対応準備をし、感染症例について役所の公衆衛生担当部署と定期的に確認を取ろう。間もなくその地域や教会が「赤信号」ゾーンに移動する可能性もある。
Be hypervigilant, and check regularly with your local public health department about additional cases that could move your community and church into the “red light” zone.
直近の旅行歴や感染者との接触歴がない感染者がコミュニティー内で確認されれば、すぐに教会は「赤信号」ゾーンに移動する。この状況が意味するのは、それまで確認されていなかった感染者がコミュニティー内に存在していたということであり、強い警戒が必要だ。疫学ではこれを「コミュニティー感染」と呼ぶ。コミュニティーにいる広い世代の感染者が外部の感染者と接触していたことが分かった場合も、その教会は「赤信号」ゾーンに入る。「赤信号」ゾーンの教会はすぐに次の対応を取る必要がある。
Your church moves into the “red light” zone as soon as a resident of your community becomes infected but has not traveled recently to another area with cases and cannot be linked to any other case. This raises alarm because it means transmission in the community was previously undetected. Epidemiologists call this community transmission. A community is also in the red zone when multiple generations of transmission in the community are linked to an imported case. As soon as you are in the red zone, your church should do the following:
●さまざまな「人との距離を確保する対策」を実施し、身体的に弱いグループを保護しよう。
Implement various social distancing measures and protect the vulnerable groups.
●コミュニティー感染が広がっていれば、礼拝を含む活動の中止範囲を広げ、可能であればオンライン礼拝や小グループでの礼拝に移行すべきだ。
As more community transmission takes place, temporarily discontinue more and more activities, including corporate worship, and move if possible to livestreaming or to small group worship.
●地域行政の公衆衛生担当部署からの警告や勧告に注意しよう。集会を制限するよう求められる場合もある。
Watch for recommendations or mandates from your local public health department; you may be asked to limit social gatherings.

ほとんど空のスーパーマーケットの棚。オーストラリアのメルボルンで(写真:Christopher Corneschi)
教会の活動を決定する方法
How to make decisions on your church’s activities
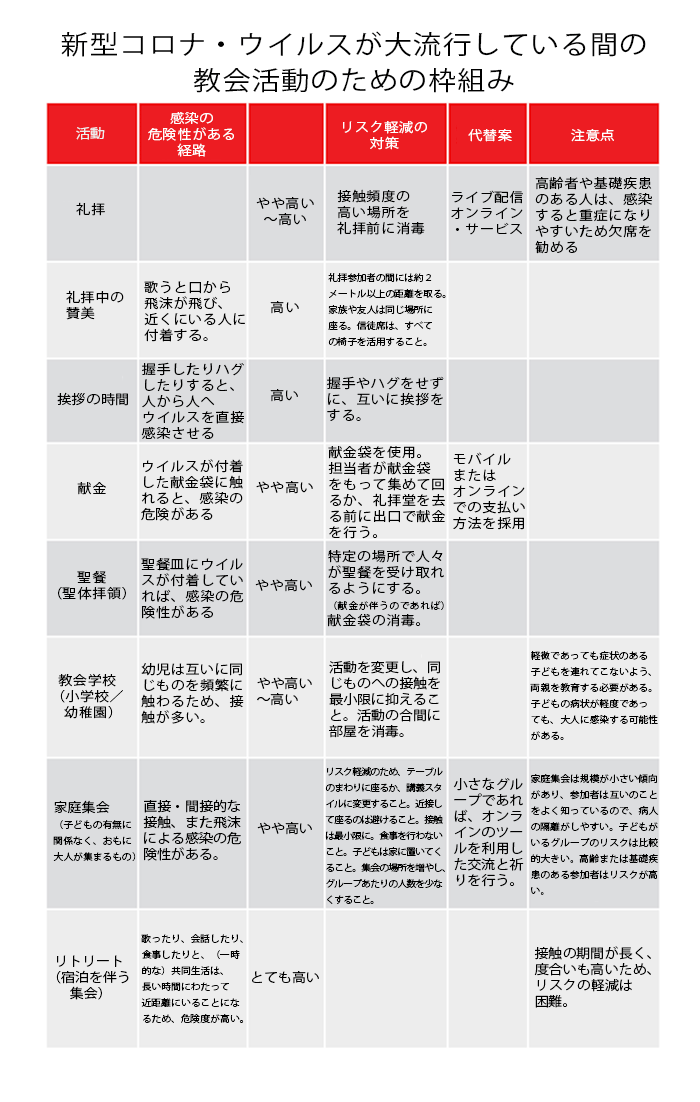
シアトルにある3つの教会と協働する中で分かった苦労は、新型コロナ・ウイルスへの対策として計画の中止や変更を発表した時に出てくる、さまざまな反応への対処だ。私はその手助けとなる枠組みを考案した。これは表(スプレッドシート)を利用して、教会の活動をリストにまとめ、それぞれの活動にウイルスがもたらす影響の可能性を考え、そのリスクを評価し、修正案や代替案をあらかじめ設定しておき、それぞれについて決定を下すというものだ(下図を参照)。
In my work with the three churches in Seattle, I found that they all initially struggled with diverse opinions about what activities to cancel or modify when planning their response to COVID-19. I developed a framework to help them. Using a spreadsheet, we listed church activities, thought of possible transmission of the virus during each activity, rated risks, provided modifications or substitutes, and then made decisions for each (see figure for an example).
重要なのは、それぞれの活動を通して(直接にしろ間接にしろ)どのような感染がありうるかを把握することだ。そのためにも、新型コロナ・ウイルスの感染経路を頭に入れておく必要がある。直接感染のリスク評価には、次のようなことを考えよう。人々が咳やくしゃみなどをすることで、ほかの人に飛沫感染をさせる可能性はどの程度か。手などで人と人が直接的に接触する可能性はどの程度か。歌うこと、非常に近い場所で話すこと、握手すること、ハグすることなどの活動はリスクを高める。リスクを減らすには、人と人の間の距離を約2メートル以上離すようにしたい。
The key is to work out the how transmission, whether direct or indirect, can occur through each activity. Keep in mind the ways COVID-19 is transmitted. When assessing the risk of direct transmission, ask: How likely are people to cough, sneeze, or generate respiratory droplets toward others? How likely is direct hand contact? Activities like singing, talking at very close quarters, giving handshakes, and hugging will have increased risk. To decrease risk, consider increasing distance between people, preferably to more than six feet.
間接感染のリスク評価には、次のようなことを考えよう。感染の可能性があるものに人が触れる可能性はどの程度か。献金袋や聖餐用の皿、聖書、コーヒーメーカーなど、そのものの表面に触れることを伴う活動はリスクを高める。リスクを減らすためには、頻繁な手洗いの実施、消毒剤の使用を実践しよう。
When assessing the risk of indirect transmission, ask: How likely will people touch surfaces that could be infected? Activities that involve touching surfaces, such as offering plates, Communion plates, Bibles, and coffee dispensers will increase risk. To decrease risk, implement frequent hand-washing and use of hand sanitizers.
どの活動を中止・変更するかを考える時には、対象となる年齢層を考えよう。高齢者や基礎疾患を持つ人々は、感染によるリスクがはるかに高いため、優先的に保護する必要がある。
Consider the age groups involved when planning what activities to modify or cancel. The much higher risk of severe illness among the elderly and those with chronic illnesses means we need to protect this group from infection.
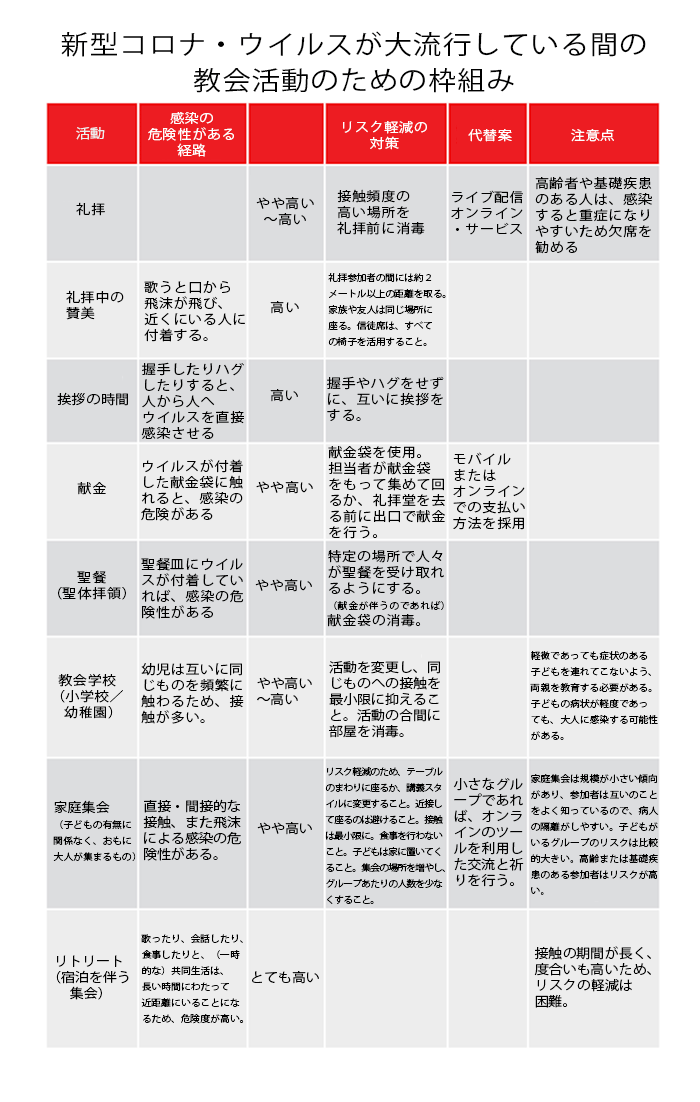
教会がどの活動を修正・中止・変更するかは、コミュニティー感染の度合いに大きく依存することを覚えておこう(上図を参照)。度合いが低い場合、一部のプログラムを変更するだけで、中止はしなくてもいい。しかし、コミュニティー感染の度合いが上がれば、感染したことを知らない人が教会に来る可能性が高まるため、活動は中止したほうが賢明だ。行政の公衆衛生担当部署が推奨する対策にも従ったほうがいい。
Remember, the decision of what church activities to modify, cancel, or substitute largely depends on the level of community transmission (see figure). If the level is low, you may just modify some activities but not cancel any. But as the level of community transmission increases, canceling activities becomes a better idea because it is increasingly likely that an infected person will enter the church unknowingly. Finally, follow public health recommendations.
このアプローチの採用を決めたある牧師は次のように述べた。「子どもたちは常に触り合っており、コントロールすることはできないため、子どもたちへのミニストリーはリスクが高いと判断しました。子どもたちが感染すれば、両親や祖父母に感染を広げてしまう可能性があります。また、教師の多くが高齢者でリスクが高いことから、すぐに子どもたちの教会学校を閉鎖することに決めました」
When using this approach, a pastor said, “We determined that children’s ministry was high risk because kids are constantly touching each other and we can’t control it. If they spread infection among themselves, they can bring it home to their parents and grandparents. Besides, many of our teachers are elderly, and we don’t want them to get infected. So, we quickly decided to close children Sunday school.”
ある長老はこう語った。「私たちの聖歌隊にはあらゆる年齢の人々が参加しています。しかし、リハーサルや礼拝で列になって歌うと、感染のリスクは中から高レベルになります。特に聖歌隊には高齢のメンバーもいるため、聖歌隊全員ではなく、カルテット(4人合唱)に変更しました」
An elder said, “Our choir had people of all ages participating. But with singing during rehearsals or when standing in rows and singing during worship, there was a medium-to-high risk of transmission. So, we decided to substitute the choir with a quartet, especially since some choir members were elderly.”
ある主任牧師は次のように述べている。「私は各部門のリーダーから、活動をどうするかの相談を電話やメールで受け取っていました。予定していた活動のリスクを別の活動リスクと比較することはたいへん有用でした。この方法では、すべての活動をリスト化することで、それぞれの感染リスクが一度に確認できます。そのおかげで一つ一つの活動について決定を下す際に一貫性を保つことができ、判断の理由を明確に伝えることができました。この方法は私たちのチームにとって大きな助けとなりました」
An executive pastor said, “I was getting calls and emails from individual ministry leaders about what to do with their activities. It was really helpful to list all the activities and review their risk of transmission all in one go because we could compare the risk of one activity to that of another. This helped us to be consistent when making decisions about individual activities, and we were able to clearly communicate why we made these decisions. That was so helpful to our team.”
教会としての対策を練る時は、教会員と連絡を密にするようにしよう。教会が計画を立てていることを知れば、安心する教会員もいる。教会の判断プロセスがどのような理論的根拠に基づいているかを理解し、それが正しい科学に基づいていることを知ることは、安心感を与える。多くの場合、判断は瞬時に行われる必要がある。教会員たちに明確かつ効果的にその情報を伝えるためにも、連絡の方法を確立しておいたほうがいい。
When developing your church’s response plan, communicate with church members. Some members’ anxiety will decrease when they know that your church is making a plan. They can better understand the rationale behind the church’s decision process and take comfort knowing it is based on good science. Develop a communication process because decisions often have to be made in real time and then clearly and effectively communicated to the congregation.
あなたの教会も、今すぐ対策を立てる必要がある
Your church needs to have a plan to respond now
過去数週間のシアトルでの経験を振り返ると、この疫病が拡大した速度に驚きを覚える。新型コロナ・ウイルスは、多くのコミュニティーに素早く甚大な被害を与えている。時間の猶予はない。私たちの教会の活動はウイルス感染を促進する可能性があり、私が医学部で教えられたように「まず被害を広げない」ための対策を取る必要がある。このウイルスについて現状分かっている情報に基づいて作られた上記のツールを利用すれば、私たちの教会は、身体的な弱さを抱える人や自らを迅速に保護するための対策を立てることができる。その計画を実行することで、私たちの教会はこの流行の拡大を食い止める大きな役割を果たし、社会の被害を減らすことができる。
Reflecting on our experience in Seattle over the past weeks, I am struck by how fast this outbreak took off. COVID-19 is going to hit many communities hard and fast. There is no time to waste. Because our church activities can facilitate the transmission of this virus, our churches should “first do no harm,” a dictum I learned in medical school. Using the tools described above, which are based on our current understanding about this virus, our churches can have a response plan in place to quickly protect ourselves and the most vulnerable among us. By implementing such a plan, our churches can play a major role in stemming the tide of this epidemic and reduce its harm on society.
ここで述べたアプローチは、公衆衛生や疫学に基づいた判断を行うことに重きを置いている。そのため、ウイルスに感染して激しい苦しみの中にある人々に共感すること、関わり合うことには重きを置いていないと言える。教会の人々が、ウイルスがどのように広がり、被害を与えるかを理解した上で、病気の人々や身体的に弱い人々のことを配慮し、世界のニーズに応えられるよう、このアプローチを改良してくれることを願っている。
The approach discussed here is admittedly heavy on good public health and epidemiological approaches for decision making but light on empathetic response and engagement around those who have the virus and are suffering from its more potent effects. I hope that, having understood how the virus spreads and harms, this response plan can also include ways to serve with compassion those who are sick, care for the most vulnerable, and become a congregation more sensitized to and engaged with the needs of the world.
執筆者のダニエル・チンは、25年にわたる世界的な公衆衛生の経験を持つ医師。専門は肺、救命救急および疫学。
本記事は「クリスチャニティー・トゥデイ」(米国)より翻訳、転載しました。翻訳にあたって、多少の省略をしています。
出典URL:https://www.christianitytoday.com/ct/2020/march-web-only/seattle-churches-stop-meeting-to-slow-covid-19-coronavirus.html
「クリスチャニティー・トゥデイ」(Christianity Today)は、1956年に伝道者ビリー・グラハムと編集長カール・ヘンリーにより創刊された、クリスチャンのための定期刊行物。96年、ウェブサイトが開設されて記事掲載が始められた。雑誌は今、500万以上のクリスチャン指導者に毎月届けられ、オンラインの購読者は1000万に上る。
関連