注:以前の記事では「集会中に歌うのはやめるべき」と誤解されるような記述がありました。著者が意図している提案は、「歌ったり話したりする時はマスクを着用すること」です(詳細については、本記事中の表を参照)。
Editor’s Note: An earlier version of this article implied that people should not sing during gatherings. The author’s suggestion is to wear a face mask when singing or talking. (See updated table for more information.)
この4カ月で、新型コロナ・ウイルスは世界中で爆発的に広がった。緊急治療室はいっぱいになり、集中治療室には人工呼吸器をつけられた患者が並び、愛する人を失った多くの家族が悲しみに暮れている。ウイルスの蔓延(まんえん)を抑えるために、ほとんどの政府は厳格な在宅命令を下している。このような画一的な対応が必要となったのは、多くの国がこのウイルスの急速な拡大に備えていなかったためだ。もしそのまま放置していたら、感染者の増加で医療システムは崩壊し、死者は激増したことだろう。
Over the past four months, the spread of a new coronavirus has exploded across the globe, leaving packed ERs, ICU patients on ventilators, and families grieving over the loss of their loved ones. To limit the spread of this virus, most governments implemented strict stay-at-home orders. This very blunt instrument was necessary because many countries were simply unprepared for the rapid spread of this virus. If nothing was done, the rising number of infections would have overwhelmed health care systems, and deaths would have quickly escalated.
この間、世界中の多くの教会は、顔を合わせての礼拝や宣教活動を休止した。ほかの予防措置と同じように、礼拝の休止によって新型コロナ・ウイルスの蔓延がどれほど軽減されたのか、私たちには知るよしもない。しかし、25年にわたって世界中の疫病を抑制するため尽力してきたグローバル・ヘルスの専門家である私は、この対策によって多くの礼拝出席者やその家族、友人の感染や死亡が防がれたと確信している。
During this period, churches across the US and around the world have closed their doors to in-person worship and ministries. As with many preventive actions, we may never know how this has limited the spread of COVID-19. But as a global health professional who has worked for 25 years to control diseases around the world, I am certain that this has prevented many infections and deaths that would have occurred among congregants and their families and friends.
米国で在宅命令が出されたここ6週間以上の間、失業者の数は急速に増え、多くの人が自宅でのストレスに苦しんでいる。規制緩和を政府に求める声は大きくなる一方だ。
After six or more weeks of stay-at-home orders in the US, unemployment claims are piling up, people are getting antsy in their homes, and loud voices are increasingly calling for governments to relax their restrictions.
公衆衛生の専門家たちは、「パンデミックを抑制するために必要な検査や感染経路の追跡、および検疫の体制が米国には不十分だ」と警告しているが、一部の州ではすでに制限が緩和されており、「(市民生活に)必要不可欠ではない」企業にも営業再開許可が与えられている。
Public health experts warn that the US lacks the testing, contact tracing, and quarantining capabilities needed to bring and keep the pandemic under control, yet some states are already loosening their restrictions and allowing “nonessential” businesses to reopen.
私たちの教会はいま難しい判断を迫られている。顔を合わせての教会活動をいつ再開するのか、そしてどうすればその活動を安全に行えるのか。
Our churches are now facing a set of difficult decisions: when to resume in-person ministries and how to carry out these ministries safely.
今後、世界中の教会がその使命を果たし、教会員の必要を満たしつつ信徒と地域の人々の命を守るために、安全対策を段階的に移行させることを私は勧めたい。
I propose that the way forward is to take a step-by-step approach that helps the global church live out its missional calling, meet the needs of its congregants, and protect the health of those in the church and in the community.
判断を下すための道しるべ
Our guideposts for decision-making
私がシアトルで奉仕している教会に対して「神は何を呼びかけられているのか」と考えるとき、「聖書の真実」と「科学的知識」という二つの指針に頼った。それはどちらも神から授かったものだ。
To discern God’s call for the churches I am advising in my city of Seattle, I have relied on two guideposts: biblical truths and scientific knowledge, both of which have been given by God.
大宣教命令は私たちに、「あなたの神である主を愛しなさい。……隣人を自分のように愛しなさい」と命じている(マタイ22:37~39)。コロナ大流行の中で分かったのは、「自分自身を愛する」とは「自らの身を感染から守る」ということだ。同じように私たちは、「隣人の身を感染から守る」ことによって「隣人を愛する」ことを証ししなければならない。
The Great Commandment states, “You shall love the Lord your God … and love your neighbor as yourself” (Matt. 22:37–39, ESV). During this pandemic, love for ourselves is expressed in the ways we protect ourselves from getting infected. In the same way, love for our neighbor is expressed in the ways we protect them from getting infected.
新型コロナ・ウイルスの感染防止を考えるとき、自分や他者の精神的・感情的・社会的なニーズを無視してはならない。社会的距離をとるこの時代、教会がそういったニーズを満たす必要性はむしろ高くなっていると言えるだろう。
Even as we focus on preventing COVID-19 infections, however, we should not neglect spiritual, emotional, and social needs—in ourselves and others. During this period of social distancing, it is perhaps even more important that churches meet these needs.
キリストの弟子である私たちは、礼拝、祈り、励まし、証し、弟子、奉仕という自らの召しを通して、これらのニーズを満たすことができる。一方、新型コロナ・ウイルス感染リスクを最小限に抑える方法でそれらを実行する責務が私たちにはある。このウイルスに関する科学的知識を生かしつつ、教会がクラスターになるような事態を防がなければならない。
As Christ’s disciples, these needs are met as we live out our calling to worship, pray, encourage, witness, disciple, and serve. However, we now must do these in a way that minimizes the risk of COVID-19 transmission. Therefore, we need to use scientific knowledge about this virus to prevent its spread in our churches.
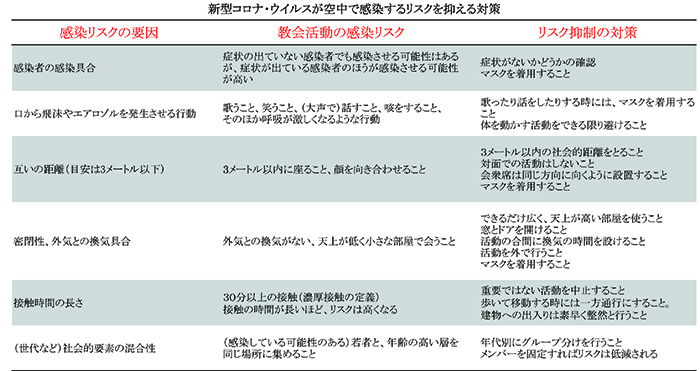
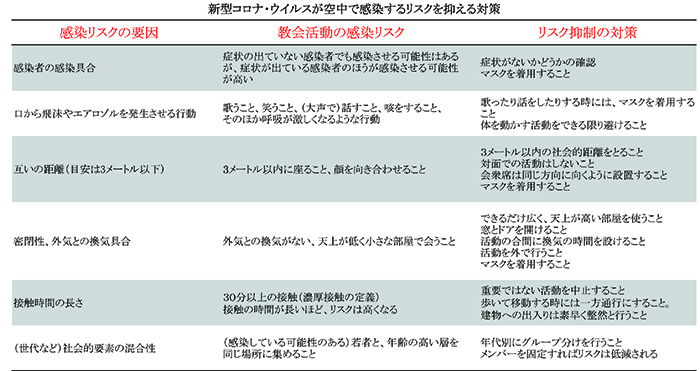
表1
新型コロナ・ウイルスについての最新の科学的知識
Recent scientific knowledge about COVID-19
現在、世界中の優れた人々が解決に取り組む中で、このウイルスについての科学的情報が急速に集められている。また、この疫病の拡大抑制には「何が効果的で、何が効果的でないのか」という情報も、各国での教訓から共有されている。「顔を合わせての教会活動をこれからどう再開するか」を考えている人にとって、関連性の高い情報も得られている。
With the best minds in the world working on COVID-19 right now, there is a rapidly expanding body of scientific knowledge about this virus. We are also accumulating lessons from many countries on what is and is not working to control the spread of COVID-19. Some of these recent insights are particularly relevant to churches as they consider how to resume in-person ministries:
1 ウイルス感染の仕方
First, we have a better understanding about how the virus spreads.
私たちが当初想像したものとは違い、新型コロナ・ウイルスは発症前に感染する可能性があることが明らかになった。そういうわけで、このウイルスがなぜ簡単に、しかも密かに拡散するかが分かったのだが、一方、その抑制方法は非常に複雑なものとなっている。
Contrary to our initial assumptions, we now know that COVID-19 can be transmitted before a person develops symptoms. This explains why the virus spreads so easily and stealthily, and it greatly complicates efforts to contain its spread.
また、すべての感染者が他者に感染させるわけでないことも分かっている。感染には次のような要因が関連している。
・感染者の感染具合
・口から飛沫(ひまつ)およびエアロゾルが空気中に放出される頻度
・感染者からの距離(3メートル以内はリスクが高いと考えられている)
・どれだけ外気との換気があるかという密閉環境
・感染者と過ごした時間の長さ
・世代などの社会的要素がどれだけ混合しているか
We also know that not every infected person will infect another person. Other factors are needed to facilitate transmission. They include:
・Infectiousness of a COVID-19 patient
・Actions that increase the release of respiratory droplets and aerosols into the surrounding air
・Proximity to an infected person (within six feet is considered high risk)
・Enclosed environment with limited ventilation to the outside
・Amount of time spent with an infected person
・Type of social network, e.g. inter-generational mixing
これらの要因が多いほど感染リスクは高まるし、逆に要因を減らせば感染リスクは低くなる(上の表を参照)。
The more these factors are present, the higher is the risk of transmission. But the more we can mitigate these factors, the lower the risk of transmission. (see table below).
若い人や子こどもが新型コロナ・ウイルス感染症にかかりにくいという証拠も増えている。また、子どもは感染しても症状が出る可能性が低い。ただし、体内に蓄積するウイルスの量や他の人に感染する可能性の高さは変わらないようだ。そのため、感染リスクが高い高齢者は世代間の接触を最小限に抑える必要がある。
There is growing evidence that younger people and children are less susceptible to COVID-19. Children are also less likely to display symptoms when infected with the coronavirus. However, the quantity of viruses they harbor and their ability to spread to others may not be different. Because older people are more susceptible to getting COVID-19, the implication is that intergenerational contact should be minimized to reduce COVID-19 transmission.
2 新型コロナ・ウイルスのもたらす健康被害
Second, we know much more about harmful effects of COVID-19.
当初、新型コロナ・ウイルスの危険性について、致死率の高い高齢者にばかり注意が向けられていた。その後、高血圧や糖尿病などの一般的な慢性疾患があれば、若い人でも深刻な合併症のリスクが高いことが分かった。米国で新型コロナ・ウイルス感染症にかかって入院している60%近くは65歳未満だ。
Initially, most of the attention about the danger of COVID-19 focused on the elderly because they have a much higher case-fatality rate. Then we learned that younger adults with common chronic conditions like hypertension and diabetes also have an increased risk of serious complications. In fact, nearly 60 percent of COVID-19 hospital admissions in the US are for those less than 65 years old.
最近の研究では、米国の成人のうち45%が深刻な合併症のリスク要因を抱えていると報告された。平均的に言って、教会に通う人は年配者が多く、合併症のリスクと合わせると、教会に来る層のリスクは総じて高いといえる。
A recent study reported that 45 percent of American adults have factors that place them at risk for serious COVID-19 complications. Because those attending churches are on average older than the general population, an even higher proportion of church congregants are at risk for serious COVID-19 complications.
3 どんな手段が有効か
Third, we have a better understanding of what control measures work.
検査、感染経路の追跡、検疫により、大規模なロックダウンをせずとも新型コロナ・ウイルス蔓延を緩和させることは可能だ。ただしそのためには、スピーディーに対策をとる必要がある。発症から2〜3日以内に検査を行い、その接触者の隔離を実施した韓国と台湾はその好例だ。韓国と台湾が成功したのは、世界的に見ても検査率が高く、感染経路をすばやく見つけて検疫を実施する体制が整えられていたからだ。電子情報を用いた情報追跡を行ったことも大きな要因だが、それは(人権が重んじられている)他国では不可能だったかもしれない。
Testing, contact tracing, and quarantining of cases and contacts can mitigate the COVID-19 epidemic without a major lockdown. However, such actions must be taken very rapidly and effectively. South Korea and Taiwan have done this successfully. Within two or three days from symptom onset, COVID-19 patients are tested and most of their contacts are effectively quarantined. This has worked because South Korea and Taiwan have some of the highest testing rates in the world and a well-trained cadre of contact tracers to quickly locate contacts and implement quarantine. They also use some electronic tracking, which may not be acceptable in other countries.
咳(せき)をしたり、大声を出したりすることで発生する飛沫やエアロゾルを抑えるには、マスクの使用が有効なことも分かっている。マスクの大きな利点は、感染者から他の人に感染するリスクを低減できることだ。医療用マスクと比べると効果は落ちるものの、手作りマスクにも効果はある。またマスクを着用すれば、感染者が鼻をこすったりして肌にウイルスが付着することも防ぐことできる。完全ではないものの、他者からの感染を防ぐ効果もある。
There is good evidence that using a face mask substantially reduces the release of respiratory droplets and aerosols into the surrounding air, even when a person coughs or shouts. The primary benefit from using a face mask is to reduce the spread of COVID-19 from the source of infection—an infected person. Homemade masks are less effective than surgical masks but still helpful. In addition, wearing a face mask prevents an infected person from rubbing her nose and then depositing viruses on surfaces that she touches. Face mask users also get limited protection from COVID-19 infection.
4 当面の間、新型コロナ・ウイルスは存在し続ける
Fourth, experts agree that COVID-19 will be in the US for the foreseeable future, with fluctuating levels of infection in the community.
米国には多くの感染者数が確認され続けている州や、感染者数が減り始めたばかりなのに在宅命令が解除され始めた州があり、そうした州では感染リスクと感染者数の増加が懸念される。大規模な検査の実施や効率的な感染経路の追跡、接触者への検疫を実施すればそのリスクも軽減できるが、そのような対策を行えるほどの準備や、訓練を受けた人員の確保が十分にできている州はまだない。
Several states have started to lift stay-at-home orders, even though their COVID-19 case counts remain high or have just started to decline. This will lead to an increase in transmission and new cases. This increase can be mitigated by extensive testing, effective contact tracing, and quarantining of contacts. But no state yet has the testing capacity and the trained personnel to carry out effective tracing and quarantining.
また、「地域間の感染拡大」という課題もある。自分の地域で感染者数が大幅に減少したとしても、ほかの地域でパンデミックが起こっている限り、そこから再び感染が拡大するという可能性は残されている。同様に、他国から感染が流れ込んでくることもある。その最たる例は、中国からの感染拡大を防いだものの、ヨーロッパからの感染第二波を経験したシンガポールだ。
Then there is the challenge of COVID-19 spreading from one state to another. As long as one part of the country has a poorly controlled epidemic, states that have significantly reduced their cases will remain vulnerable to COVID-19 spread from those areas. The same can be said of spread from one country to another. A prime example of this is Singapore, which controlled the first wave of infection from China only to experience a second wave of infection from Europe.
科学に基づいた計画を立てる
Making a science-based plan
教会が行う多くの活動には、空中を通した感染が起こる要因があり、教会には高い感染リスクがある(上の表を参照)。また多くの信徒は、深刻な合併症を引き起こしうる要因を抱えている。したがって教会は、顔を合わせての教会活動をいつ、どのように再開するかを慎重に検討し、その計画を明確にする必要がある。計画を立てる際には、次のことに注意したい。
The church is a high-risk setting for COVID-19 transmission. Church activities contain multiple factors that facilitate airborne COVID-19 spread (see table below). In addition, our congregants are at greater risk for serious complications from COVID-19. Therefore, churches should carefully consider when and how to resume in-person ministries and have a clear plan to do so. This plan should achieve the following:
・教会活動によって、新型コロナ・ウイルスが空中で感染するリスクを軽減させること
・その地域での感染者数の推移に併せて、教会活動の程度を調節できるようにすること
・必要に応じて、感染者との接触経路の特定を支援すること
・その地域で明らかに感染者が減少したことが証明できるまでは、顔を合わせての教会活動を再開しないこと(後編に続く)
・Mitigate the risk of airborne COVID-19 transmission during church activities.
・Be able to dial up and dial down church activities as COVID-19 infection in the community waxes and wanes.
・Be able to rapidly identify contacts with an infected person and help trace them if necessary.
・Resume in-person church activities only when there is clear evidence of a declining and low level of infection in the community.
「クリスチャニティー・トゥデイ」(Christianity Today)は、1956年に伝道者ビリー・グラハムと編集長カール・ヘンリーにより創刊された、クリスチャンのための定期刊行物。96年、ウェブサイトが開設されて記事掲載が始められた。雑誌は今、500万以上のクリスチャン指導者に毎月届けられ、オンラインの購読者は1000万に上る。
関連